Find Support to Help Your Child Overcome Depression at Artemis
In recent years, severe depression in children and teens has been on the rise in the United States, with Arizona being no exception. While child and adolescent depression symptoms may be similar to those of adults, it takes a specific mental health professional to treat depression in young people effectively. An effective teen depression treatment center provides a structured environment to facilitate healing.
Artemis Adolescent Healing Center in Tucson, Arizona, specializes in adolescent psychiatry. We recognize adolescent and adult differences, ensuring that we treat teen depression and other mental health problems safely.
If you’re a parent searching for more information on teen depression symptoms and evidence-based treatment options, read on. This page will help you understand depressive symptoms, different types of teen depression, and treatment options.
A Holistic Approach to Treating Teenagers’ Depressive Symptoms
Treating clinical depression in teenagers means taking a holistic approach to care. Our approach to mental illnesses recognizes how emotional, physical, and mental health conditions often connect. Why’s that important? Factors like family history and the presence of physical health conditions can be the key to resolving a teen’s mental health issues.
We also collaborate with a child’s healthcare provider to develop tailored treatment plans. This integration ensures we meet each adolescent’s unique needs.
Based on our assessment and initial management, we create a holistic, customized strategy for each teen. It’s often a blend of talk therapy, alternative treatments, and, sometimes, antidepressant medications.
Get Confidential Depression and Trauma Assessment
Major Depressive Disorder in Teens: A National Problem
Let’s start by reassuring parents that while the stigmatization of mental health problems makes you feel isolated, you are not alone. Major depression symptoms impact a large number of teenagers in the United States, but many people handle it quietly and with little support.
The National Institute on Mental Health (NIMH) reports that adolescent depression impacts roughly 5 million American teens aged 12 to 17. That number represents 20.1%, approximately 1 in 5 teens. Depression is higher in females at 29.2% than males at 11.5%.
That number matches Arizona’s 24% statewide statistics on Adverse Childhood Experiences or ACES. ACEs factors include living in poverty, parental neglect, or witnessing violence. These are known risk factors underlying the development of several mental disorders, including depression.
Types of Depression in Teens and Young Adults
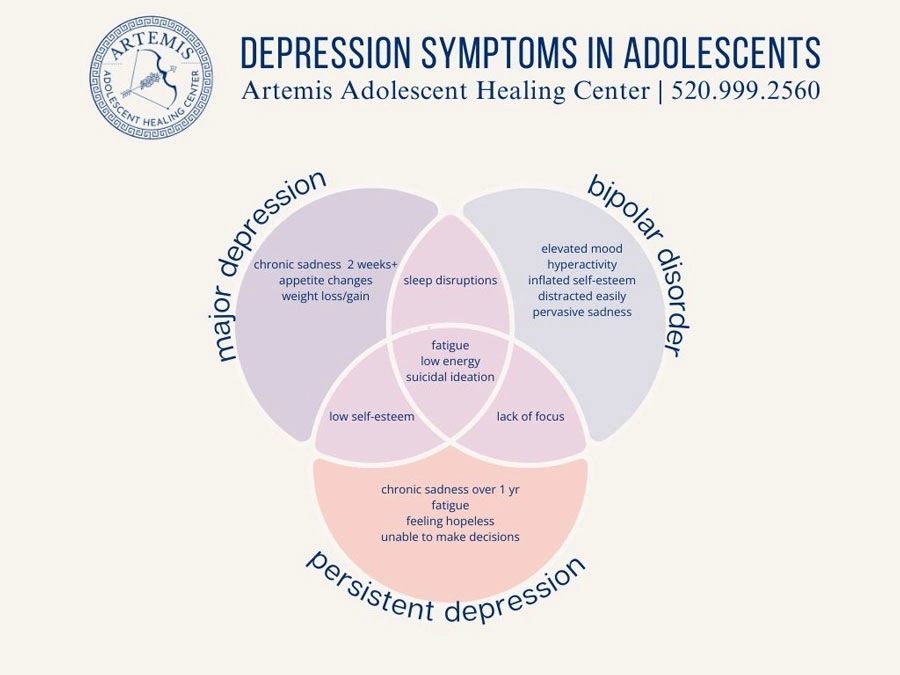
The Cleveland Clinic explains that child and adolescent depression is a mood disorder that can cause them to feel sad to the point of disrupting their typical daily activities. When sadness seems ongoing and unrelenting, it’s time to seek help. An expert in adolescent psychology can diagnose the specific depression.
Major Depression in Teens
Major depressive disorders are the most common in teens. They experience at least 2 weeks of intense sadness and irritability. The symptoms disrupt their daily function and may lead to lower grades if left untreated.
Signs of Major Depressive Disorders in Youth
Watch for these symptoms of MDD:
- Continuous sadness
- Withdrawal from friends and family members
- Loss of interest in fun activities
- Sleep disruptions
- Changes in appetite or weight
- Expressing feelings of guilt or worthlessness
- Suicidal ideation
Take these symptoms seriously. Most kids experience these problems but improve within two weeks. Episodes lasting two weeks is a sign they need a professional evaluation.
Bipolar Disorder in Youth
Bipolar disorder can occur in childhood. Some parents are surprised to hear that children can experience the mood swings of bipolar. Some mental health professionals treat bipolar depression in children without an official diagnosis because the symptoms overlap with other psychiatric disorders.
Bipolar Depression Symptoms in Adolescents
Be on the lookout for these signs:
- Manic phases with unusually high energy, sleeplessness, risk-taking, “partying” with drugs or alcohol
- Depressive phases with sadness, fatigue, self-isolation, self-harm behaviors like cutting or suicidal thoughts
Seek help if you recognize these phases in your child. Early treatment is needed to help your teen enjoy life again.
Persistent Depressive Disorder
PDD, or dysthymia, is chronic depression that lasts for a year or more in teenagers and young adults. To some, it just seems like they have a low-key personality, making it easy to miss a diagnosis.
PDD Symptoms in Teens
If your teen’s symptoms look like these, it may indicate PDD:
- Low mood
- Lack of self-esteem
- Irritability
- Lack of interest in life
- Unmotivated
- Loss of interest in friends
- Difficulty with focus or concentration
With early intervention, managing depression in teens is possible.
Adolescent and Adult Differences in Depressive Disorders
Have you wondered how depression symptoms vary between teenagers and adults? Take note of these key differences:
| Adolescents | Adults | |
| Mood indicators | More likely to be irritable and angry. May develop behavioral issues | Tend to have persistent sadness. More likely to become withdrawn from friends or family |
| Behavioral changes | Decline in academics; self-isolates from friends; may need more sleep; unusually sensitive to criticism. | Often develop insomnia; lower work productivity or performance; stops doing hobbies/fun activities |
| Physical differences | More prone to have unexplained headaches or stomachaches | More likely to have fatigue, unwanted weight loss, or gain a few pounds |
| Cognitive differences | Struggle to concentrate with lower grades the result; indecisive or forgetful | Thinks more slowly; indecisiveness can impact work performance |
| Suicidal ideation | Expresses suicidal thoughts indirectly by risky behaviors or discussing death; risk increases with a family history of depression | May more directly express suicidal plans; risk increases with previous suicide attempts or certain medical conditions |
Overlap between adults and teens is not uncommon, especially in older teenagers. Learning to recognize these signs of depression can help you get age-appropriate mental health intervention.
Other Teen Disorders That Require a Mental Health Professional

Besides depression, teens can have a host of conditions that cause depressive symptoms. A depressed mood can be present with any of these conditions:
Attention Deficit Hyperactivity Disorder
ADHD is a neurodevelopmental disorder that includes inattention, impulsivity, and hyperactivity. Studies show that the likelihood of having ADHD co-occurring with major depression is as high as 50%. That makes it 5 times higher than in teenagers without ADHD.
EXAMPLE:
‘Alex,’ 15, had always been described as a fireball of energy. In his mid-teens, his teachers started to notice that he struggled to stay focused during class. Despite his bright and curious mind, his grades had dropped due to incomplete assignments. Alex became snappy and withdrawn at home, often venting about his frustration.
Alex’s parents agreed to seek professional care, where he received a diagnosis of ADHD with overlapping depressive symptoms. Alex’s comprehensive treatment plan and an IEP at school has him back on track – mentally and academically. He’s hopes to find a hands-on job after he graduates and is looking into a welding apprenticeship.
Traumatic Brain Injury
TBI occurs due to external force on the brain. It can come from a sports injury, car wreck, or a hard tumble – even when wearing proper safety equipment. TBI can lead to behavioral changes and moodiness. The injury may lead to mental health disorders, including negative feelings that we most commonly attribute to depression.
EXAMPLE:
‘Ruby,’ 14, was her school’s soccer star until she suffered a concussion during a game. After the injury, her mother noticed Ruby’s lack of focus and a change in her social interactions. She also expressed uncharacteristic feelings of hopelessness. Her mother took her to a doctor, who ordered additional tests and found moderate trauma to the brain.
Ruby received a custom-tailored program to help regain cognitive function and attends outpatient therapy to address the depression. She has started playing soccer again in her backyard and is teaching her moves to her little brother.
Anxiety Disorder
Anxiety disorders, which present as excessive fear or worries, can interfere with a youth’s daily routine. Adolescents who struggle with it feel low self-worth, become withdrawn, and feel fatigued. They may appear to be depressed adolescents, so a professional diagnosis is a must.
EXAMPLE:
‘Liam,’ 17, had always been a top student. His constant worry about his grades and college prospects eventually overwhelmed him. He sometimes complained of a racing heart and shortness of breath before taking exams. Liam also fell rundown, sad, and lost interest in his model-airplane hobby.
On the suggestion of the school counselor, Liam’s father sought a professional assessment, where they learned that he had an anxiety disorder along with signs of mild depression. A therapist helped Liam learn relaxation techniques and other coping skills to manage his anxiety and stabilize his mood. His hard work paid off, and he now attends an engineering program at a top university – without anxiety.
Substance Use Disorders

Substance abuse often co-occurs with adolescent depression. They turn to substance abuse to self-medicate their symptoms to soothe the depression. It creates a complexity that requires ongoing management of both the substance abuse and the depression symptoms simultaneously.
EXAMPLE:
‘Sarah,’ 15, was often bullied and wanted nothing more than to fit in with her peers. She started drinking alcohol to fit in with the popular kids. Her casual use of alcohol escalated over time, and Sarah began taking illicit pills (blues) to continue hiding her pain. When her parents caught on to the substance use, they found professional help.
Sarah had a substance use disorder and co-occurring persistent depression. Sarah received comprehensive treatment that included counseling and antidepressant treatment. After therapy, she continued to attend SMART Recovery for ongoing community support and has learned she doesn’t need the approval of others.
Conduct Disorder (CD)
Adolescents with CD can be aggressive, deceitful, or violate the rights of others. Their impulsive, risky behaviors can seem to overlap with the manic phase of bipolar disorder. However, they are distinct disorders, each requiring compassionate, comprehensive care.
EXAMPLE:
‘Ethan,’ 13, grew up in the foster care system. He started exhibiting aggressive behavior and became defiant in school and his foster home. When he got caught vandalizing a local bakery, he showed the police and judge little remorse. His frustrated caregivers coordinated with his caseworker to get a thorough evaluation. Ethan was diagnosed with a conduct disorder and depression related to his traumatic early childhood. With early intervention, including intensive therapy to address the trauma at the root of his mental health challenges, Ethan started making small steps toward positive change.
Get Effective Trauma Treatment Options
How Clinical Child Psychologists Make an Accurate Diagnosis
With so many possible affective disorders like depression, you might wonder how mental health treatment specialists make a diagnosis.
They follow the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5). These guidelines have set standardized criteria for mental health conditions. Additionally, they follow clinical practice guidelines to assess symptoms, evaluate suicide risk, and consider the comparative efficacy of all treatment options.
Taking this comprehensive approach ensures that each patient receives a precise diagnosis. Thus, the clinical team can devise individualized depression treatment options.
Therapies That Address Teen Depression

Artemis therapists will use a variety of methods to address the individual needs of a depressed teen, including a mix of the following:
Interpersonal Psychotherapy (PT)
Interpersonal therapy helps improve a teen’s social relationships and mental well-being. They address teen concerns, including grief, social isolation, and role disputes, to develop better communication and problem-solving skills. IPT is particularly helpful for teens who are often involved in conflicts with their loved ones.
Cognitive Behavioral Therapy (CBT)
Cognitive behavior therapy is an approach to healing that helps teens identify and change negative thinking patterns. As they learn to reframe their thinking, they see improved moods and can start learning new coping strategies.
Dialectical Behavior Therapy (DBT)
DBT combines CBT with mindfulness practices to help teenagers manage their emotions and reduce self-destructive behaviors. The therapy was originally for treating borderline personality disorder, but it’s been adapted in recent years to treat people who struggle with depression.
Family Therapy
In addition to the individual talk therapy methods listed above, family treatment can help address relationship problems that have contributed to the teen’s depression. A counselor can help the family learn to communicate and resolve conflicts while supporting the young person’s mental health.
Medication Management
Depressed teens may also need our clinicians to provide medication management. That term means administering antidepressant medicines at the proper dose and monitoring progress. This monitoring and follow-up is critical, as some antidepressant medications have side effects, including suicidal thoughts or suicide attempts, especially in the first few weeks of treatment.
Selective Serotonin Reuptake Inhibitors
SSRIs are a first-line medication for adolescent depression because they manage depression remarkably well. They increase the brain’s serotonin output, which improves mood. Fluoxetine treatment (Prozac) and escitalopram (Lexapro) are both approved by the United States FDA for teenage use.
Some parents inquire about alternative medicine, including herbal supplements. While herbal remedies may have some benefits, they have been far less studied than prescription antidepressant medications and can lead to side effects or drug interactions.
Managing Costs When Seeking Care for Teen Depression

Teen depression is a serious matter – one you cannot ignore; it generally worsens if left untreated. Your insurance entitles you to assessment, evaluation, and evidence-based treatment options.
If you are concerned about depression treatment costs, we urge you to call our insurance verification team. Our dedicated insurance coordinators will help you make the most of your health insurance benefits.
With our team’s help, you will understand what benefits you’re entitled to and know the estimated out-of-pocket costs before you admit your teenager to our program. In many cases, we have leveraged client benefits to cover all treatment costs.
Up To 100% of Rehab Costs Covered By Insurance
Get Help for Your Depressed Person at Artemis Today
If you are a parent concerned about the depression symptoms you’ve noticed in your teenager, Artemis is here to help. We offer a full continuum of care and will provide an accurate diagnosis and a customized treatment plan for your child’s depression.
Without treatment, depressed adolescents grow up to become depressed adults. It’s time to stop that progression in its tracks. Call us for information on how Artemis programs can help.
All calls are confidential, so please reach out for expert support options today.






